Friends and Family,
Sometimes Genevieve and I fly down to San Diego to see my oncologist, and we are full of optimism. Sure, there’s plenty of “scanxiety” mixed in because there is so much at stake, but, deep down, we get a good feeling that everything is going to go well. Other times, not so much. This was one of those other times.
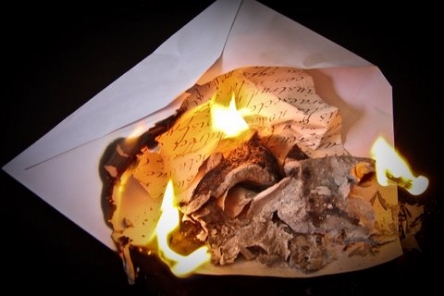
Dire Straits said it best in their song: Sometimes you’re the windshield, sometimes you’re the bug. You can find it here: https://www.youtube.com/watch?v=iAqSwUbw_v0. Before I got these last scan results, I definitely felt like the bug.
I have a cough that had been getting progressively worse for the last seven weeks. It got so bad that I was embarrassing myself at the movies. I could just stick to movies like Star Wars: The Force Awakens and other nonstop action movies so that people don’t hear me cough, but that doesn’t solve the problem, does it? Even Genevieve was admitting that she was getting worried about my cough. Genevieve’s sharing this is actually really good news as far as I am concerned, because now I can share my worries with her, and she won’t deny that there is something to worry about. I won’t feel so alone with my fears. That is a really big thing for me. There is a place for affirmations, but there also needs to be a place to accept whatever feelings come up.
That doesn’t mean that we have to live in fear, but it’s OK to visit it once in a while. I’ve learned that I’m strong enough to let the fear in, and to know that it won’t overwhelm me. Eventually, the fear gets bored and leaves. Fighting fear sucks up a lot of energy, and only makes it grow stronger. If I don’t fight it, then the fear flows in and out, just like the tide. Each time I let it in, I am able to handle it a little bit better.
A side effect of having cancer is that any minor symptom, that people without cancer wouldn’t even think twice about, could be a symptom of something more risky for me. If I have a headache for three days in a row, I wonder if the cancer has metastasized to my brain. If my back gets sore, I wonder if the cancer in my spine is spreading. And if I have a cough, it’s hard not to imagine that the cancer is taking over my lungs. When that cough keeps getting worse… Well, then. Bug, meet windshield.
It turns out that this time it WAS a bug. More specifically, it was a cold symptom that wouldn’t go away all this time. My CT scans showed no growth of the cancer again! Genevieve and I went from elation, to exhaustion, and then back to elation again. Woohoo!
And after all of that, we went back to gratitude. I am grateful that the Tagrisso / AZD9291 is still working. I’m grateful that the clinical trial for the next clinical trial drug that could help me, EGF816, will be available through clinical trial at UCSD, though I don’t know the timing yet. And I am grateful for your love and support, which is surely keeping me alive.
I’m also grateful that, at least this time, I’m still the windshield.
Love,
Dann
*** A Special Request***
I'm participating in an event to raise money to fight lung cancer - and I need your help!
I'm planning to attend LUNGevity Foundation's National HOPE Summit in Washington, DC, in May - it's a special conference just for lung cancer survivors like me. If I can raise $1000 or more in donations, LUNGevity will cover my travel expenses, including US round-trip transportation and hotel accommodations.
Proceeds from this fundraiser will benefit LUNGevity Foundation, the leading private provider of research funding for lung cancer. LUNGevity Foundation is firmly committed to making an immediate impact on increasing quality of life and survivorship of people with lung cancer by accelerating research into early detection and more effective treatments, as well as providing community, support, and education for all those affected by the disease.
If you wish to donate, please go to my LUNGevity page: http://lungevity.donordrive.com/index.cfm?fuseaction=donorDrive.participant&participantID=15681